- Lifestyle
- Health & Families
There are fewer treatment options for even routine thrush infections
Manal MohammedThe ConversationMonday 01 December 2025 15:46 GMTComments
 CloseRelated: Animal poo could 'help kill antibiotic-resistant bacteria' for NHS patients
CloseRelated: Animal poo could 'help kill antibiotic-resistant bacteria' for NHS patients
Sign up to our free Living Well email for advice on living a happier, healthier and longer life
Live your life healthier and happier with our free weekly Living Well newsletter
Live your life healthier and happier with our free weekly Living Well newsletter
 Email*SIGN UP
Email*SIGN UPI would like to be emailed about offers, events and updates from The Independent. Read our Privacy notice
Thrush is one of the most common infections in the world. It’s caused by the fungi Candida – specifically, the yeast Candida albicans.
Although yeast infections are normally treated easily with antifungal drugs, a growing number of Candida species are developing resistance to these drugs – including the species that causes thrush.
According to the US Centers for Disease Control and Prevention, about 7 per cent of all Candida blood samples tested are resistant to the antifungal drug fluconazole, the first-line drug used to treat most Candida infections.
This means there are fewer treatment options for even routine thrush infections – making them more difficult to treat.
It also means that more severe Candida infections, which can occur in people who have a weakened immune system or are taking long courses of antibiotics, will become even harder to manage.
Antifungal resistance may also be contributing to the rise in recurrent thrush (thrush infections which continue to come back). This affects around 138 million women worldwide, but is expected to rise to 158 million people by 2030.
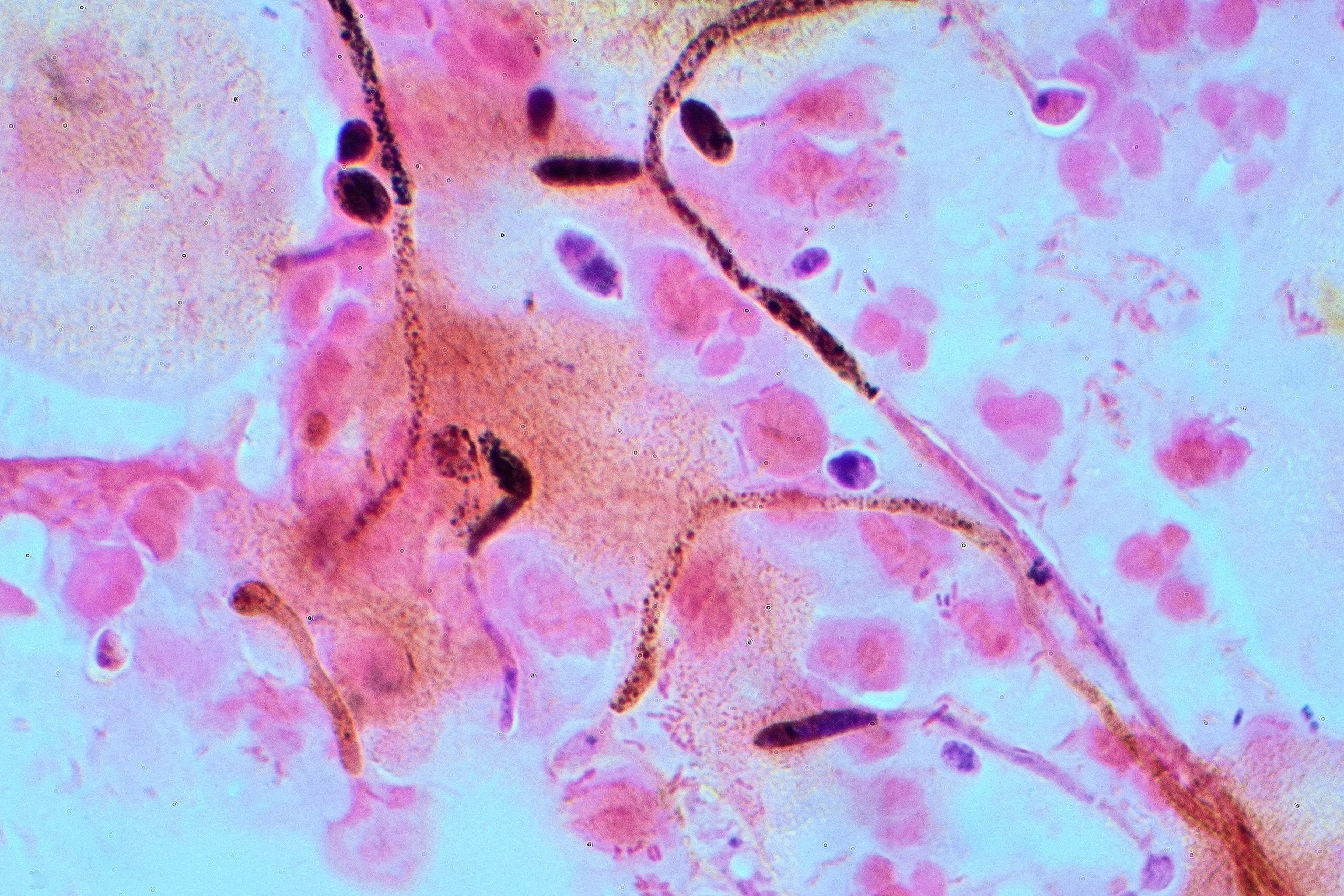 A gram stain of Candida albicans (thrush) from a vaginal swab (Graham Beards/Wikimedia Commons)
A gram stain of Candida albicans (thrush) from a vaginal swab (Graham Beards/Wikimedia Commons)Why resistance is growing
The antifungal resistance landscape has changed dramatically over the past few decades.
In the early–to-mid 2000s, antifungal resistance was rare. Fluconazole worked well for most Candida albicans infections, less than 5 per cent of which were resistant to it.
But Candida albicans is a highly adaptable microorganism, which can easily develop resistance to antifungals under the right conditions.
Research shows that resistance among Candida albicans has been trending upwards over the past eight years at least. A small study of patients in Egypt found that in 2024, nearly 26 per cent of Candida albicans isolates from blood samples were resistant to fluconazole. However, more research is needed to understand whether this picture is the same worldwide.
Candida can develop resistance to antifungal drugs through genetic mutations which make them less susceptible to antifungals, or help them reduce the drug’s effectiveness.
Candida can also protect itself from antifungal drugs by forming tough biofilms. These slimy layers of fungal cells block drugs from getting in, help the fungus pump any drugs which have penetrated the barrier back out, and allow some cells to hide in a resting state until treatment is over. Candida can also alter the structure of molecules targeted by antifungals in order to prevent the drugs from binding effectively.
About the author
Manal Mohammed is a Senior Lecturer in Medical Microbiology at the University of Westminster.
This article was first published by The Conversation and is republished under a Creative Commons licence. Read the original article.
The key reason Candida infections are becoming harder to treat is because the fungi are adapting to survive antifungal drugs. But this resistance isn’t happening by chance. There are several factors that are contributing to the problem, including misuse and overuse of antifungal drugs (not just by people but in agriculture too) and the limited number of effective antifungal drugs that are available (which are difficult and expensive to develop).
Increasing environmental temperatures, ecological stress and fungicide use are also creating conditions that favour heat-tolerant and drug-resistant Candida strains – such as Candida auris, which is highly resistant to multiple classes of antifungal drugs, and can cause severe infection in people who have a weakened immune system.
Preventing antifungal resistance
Candida is primarily transmitted through person-to-person contact, sexual contact and contact with contaminated objects or surfaces. In healthcare settings, Candida can also spread through contaminated medical equipment and devices.
Airborne transmission is not common with Candida. However, an alarming recent study reported that species of Candida resistant to common antifungal drugs were detected in urban air samples in Hong Kong. This included Candida albicans.
The presence of Candida in air could increase the likelihood of community spread and elevate the risk of inhalation – particularly in hospitals, crowded areas or care homes with immunocompromised people. This represents a potential route of exposure that has previously been underestimated. More studies will be needed to investigate where urban Candida originates and how infectious it may be.

Candida generally doesn’t cause harm under normal conditions and if you have a healthy immune system. Maintaining a healthy micriobiome is key to protecting yourself: the beneficial bacteria in your body help keep Candida levels under control and prevent it from overgrowing and becoming problematic.
However, when the balance of your friendly bacteria is disrupted – for example, by antibiotics, poor diet, a weakened immune system or high stress – Candida can grow out of control, leading to illnesses.
Microbiome disruption can also create conditions where antifungal-resistant Candida can overgrow, form resistant biofilms and become harder to treat.
Looking after your microbiome can make a significant difference in reducing the risk of Candida and other infections. This involves eating a diverse, fibre-rich diet – including fermented foods – and limiting highly processed foods.
Only take antibiotics when prescribed. Probiotics and prebiotics may also help maintain your microbiome balance, especially after antibiotic use or recurrent infections.
While most Candida infections are treatable, drug-resistant strains and infections in vulnerable people can be serious. However, we can all do our part to prevent resistant strains from developing – including by only taking antifungal medicines exactly as prescribed, completing the full course, and maintaining good hygiene.
More about
Antibioticsimmune systemThe ConversationInfectionsJoin our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments



